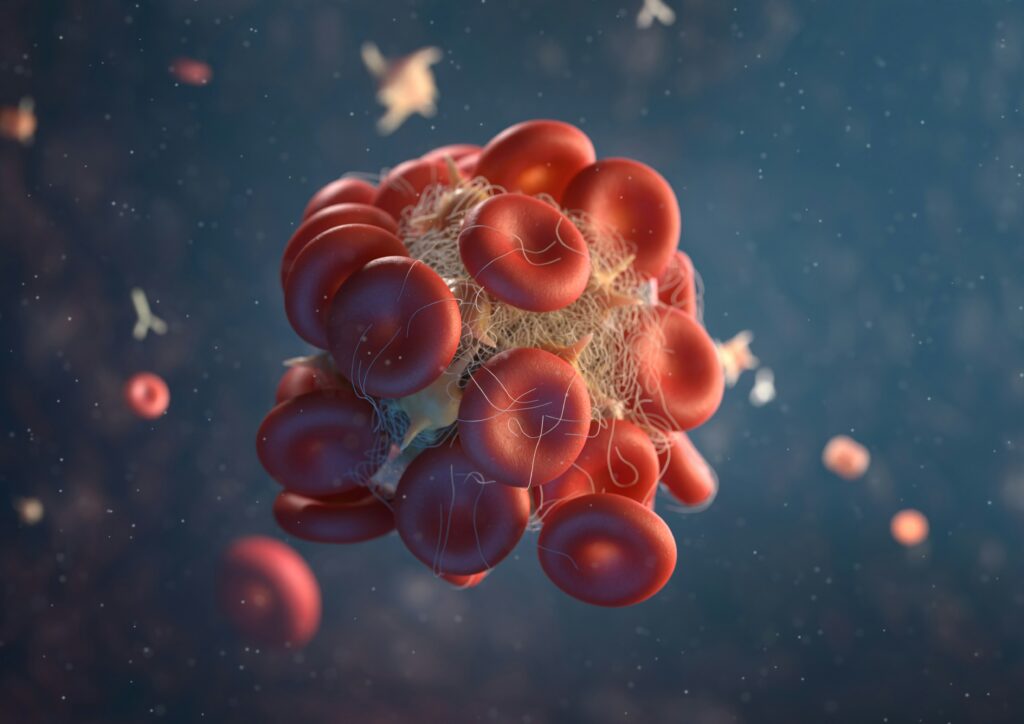
At the end of this blog we will be able to understand what are bleeding and coagulation disorders and how to mange them properly. Human body is in a constant state of balance between bleeding and clotting to maintain the normal functioning of vessels. This system is under the influence of many factors such as platelets, clotting factors and vascular endothelium. Any problem in this delicate system will either lead to bleeding disorders or coagulation disorders resulting in impairment of the body normal functioning.
Some of common tests Used For Hemostasis Are:
1. Bleeding Time: It measures time taken for a standardized skin puncture to stop bleeding. It takes about 2 to 9 minutes in a normal healthy person to stop bleeding, usually the results are below 8 minutes.
2. Platelet Count: The normal range of platelets is from 150k to 300k per micro liter. If this value is less than 150k then there is tendency for bleeding disorders.
3. Prothrombin Time: Abbreviated as PT has a normal reference interval of 9 to 12 seconds. This test is used for extrinsic and common coagulation pathway. The extrinsic factor is factor VII and the common factors are X, V, II and I.
4. Partial Thromboplastin Time: Abbreviated as PTT has a normal reference range of 26 to 36 seconds. This test is used for intrinsic and common coagulation pathway. The intrinsic factors are XII, XI, IX and VIII.
Note that If the site if bleeding is superficial then there is a defect in the platelets and if the site of bleeding is deep such as muscles and joints then there is defect in the coagulation system. Lesions formed by the platelets defects are petechial and ecchymosis while lesions formed by the coagulation defects are hemarthrosis and hematomas.

Bleeding and Coagulation Disorders:
1. Idiopathic Thrombocytopenic Purpura (ITP):
In this disease IgG antibodies are formed against glycoprotein IIb and IIIa receptors. This results in isolated thrombocytopenia with normal hematocrit and WBC count. If spleen is examined it will also be of normal size. If ITP occurs in the absence of any other known risk factor it is said to be primary ITP and if ITP is found in association with some other disease, risk factor or drug it is known as secondary ITP.
Lab Findings:
Smear results will suggest the presence of micro spherocytes. Coombs test will be positive. PT and PTT results will be normal, however bleeding time will be prolonged. Bone marrow biopsy will show increase number of megakaryocytes. ITP can be acute or chronic.
Acute ITP is commonly seen in children of age 2 to 6. It affects both the genders equally. The onset of the disease is very abrupt usually appears 1 to 3 weeks after a viral infection. Acute ITP responds well to steroids.
Chronic ITP is commonly seen in adult patients. It affects women of age 20 to 40 more than men. It is insidious in onset and does not respond to steroids.
Management:
If the platelet count is more than 30000 and there is no bleeding it requires no treatment. If the platelet count is less than 30000 and there is mild bleeding, glucocorticoids are used. If the platelet count is less than 10000 and there is severe bleeding intravenous immunoglobulin (IVIG) or intravenous Anti-Rh(D) in Rh positive individuals with glucocorticoids are given.
Splenectomy is indicated when there is chronic and refractory disease however it does not improve the problem of excessive bleeding.
Second line of therapy is used when patients after going through splenectomy still develops the disease. This regime include Romiplotism, Eltrombopag, Rituximab, Azathioprine, Cyclosporine and Mycophenolate.
2. Thrombotic Thrombocytopenic Purpura (TTP):
TTP is a vascular occlusive disease with systemic platelet aggregation. In this disease there is deficiency if enzyme ADAMTS-13 (also called vWF-cleaving metalloprotease). The enzyme ADAMTS-13 is necessary for the breakdown of Von Willebrand factor which has a very high molecular weight. Deficiency of this enzyme leads to accumulation of multimers of Von Willebrand factor in the plasma and systemic platelet aggregation.
Lab Findings of TTP:
In patients with TTP the smear test will show the presence of schistocytes. Coombs test will be negative. PT and PTT results will be normal but the bleeding time will be prolonged.
Clinical Features of TTP:
There will be thrombocytopenia and microangiopathic hemolytic anemia (MHA) leading to normocytic anemia, increased levels of LDH, increased indirect bilirubin with schistocytes. Other features include renal failure, fever and central nervous system deficits.

Management of patient with TTP:
Plasmapheresis should be done as soon as possible. Glucocorticoids should be administered. If there is delay in performing plasma exchange (plasmapheresis) then fresh frozen plasma is given. Platelet transfusion is contraindicated in TTP patients because it increases the occurrence of microvascular thrombosis.
3. Hemolytic Uremic Syndrome (HUS):
It is also a vascular occlusive disease with intra-renal aggregation.
Pathogenesis:
HUS is mediated by toxins such as Shiga toxin of O157: H7 serotype of entero-hemorrhagic E.coli. Shiga toxin has the ability to bind the endothelial cells of kidney and platelets resulting in the formation of intra-renal thrombi.
Lab Findings of HUS:
The presence of schistocytes is confirmed by smear test. Coombs test will be negative. PT and PTT will be normal with prolonged bleeding time.
Clinical Features of HUS:
There will be thrombocytopenia, renal failure and microangiopathic hemolytic anemia (MHA). This is known as the HUS Triad. MHA is characterized by the normocytic anemia, increased LDH, increased indirect bilirubin and presence of schistocytes. HUS typically affects children and is associated with bloody diarrhea caused by E.coli.
Management of patients with HUS:
Urgent plasma exchange knows as plasmapheresis should be done. If there is delay on performing plasmapheresis then fresh frozen plasma is administered. Glucocorticoids are also given to patients with HUS. Transfusion of platelets is contraindicated due to the risk of microvascular thrombosis. Antibodies are also contraindicated.
4. Heparin-Induced Thrombocytopenia (HIT):
The most common cause of thrombocytopenia in hospitalized patients especially those on heparin therapy. It is of two types.
Type I HIT: it is caused by the direct effect of heparin and is not an immune disease. It is seen in 10 to 29% of patients on heparin therapy. The symptoms starts to appear after 1 to 4 days of heparin therapy. Platelet nadir will give a result of more than 100000 per micro liter. Complications are not seen in type I. Heparin therapy can be continued under close observation.
Type II HIT is a hypersensitivity reaction mediated by IgG antibodies against platelet factor 4 with heparin complex. Seen more frequently with unfractioned heparin than LMWH. It appears after 5 days of heparin therapy. Complications include thrombosis of veins more than arteries. In such patients stop heparin immediately and start direct thrombin inhibitors like Argatroban and Bivalirudin.
What Are The Major Coagulation Disorders?
1. Von Willebrand Disease:
It is an autosomal dominant disorder with defect in gene for Von Willebrand factor(vWF). vWF binds platelets to one another and also protects factor VIII from destruction in circulatory system. Decrease in levels of vWF will result in dysfunction of platelets and decrease in factor VIII. Lab findings will show normal but defected platelet count with increased bleeding time and normal PT. PTT is increased due to decreased factor VIII. Confirmation is done by vWF mutlimer analysis.
2. Hemophilia A:
It is the most common congenital coagulation factor deficiency caused by reduced activity of factor VIII. It is X linked recessive so occurs only in males while females are silent carries of it. Hemophilia B is known as Christmas disease and is due to factor IX deficiency. There will be spontaneous hemorrhages and hemarthroses. Muscle hematomas in calf and psoas muscles. Lab results will be normal for platelet count, BT and PT but PTT will be increased.
3. Disseminated Intravascular Coagulation (DIC):
It is a thrombo-hemorrhagic disorder with massive activation of coagulation that overwhelms the normal control mechanism. Acute DIC leads to the consumption of coagulation factors and platelets leading to bleeding. Chronic DIC leads to thrombosis. DIC is caused by E.coli and Neisseria meningitis (sepsis). Obstetric complications such as placental abruption and septic abortion. Malignancies of pancreas, prostate, lung and stomach and acute promyelocytic leukemia also causes DIC. Lab reports of DIC will reveal decreased platelet count and fibrinogen while BT, PT, PTT, D-dimers and FDPs are all increased.
Conclusion:
In order to mange various diseases it is very important to understand bleeding and coagulation disorders. these disorders range from platelet dysfunction like idiopathic thrombocytopenic purpura (ITP) to coagulation disorders like Hemophilia and DIC. if these diseases are not managed properly and on time the can have fatal complications due to bleeding and thrombosis. Platelet count, bleeding time, and clotting factor analysis are helpful in early diagnosis and effective treatment of the disorders. Treatment plan differ for all these diseases, plasma exchange is done for conditions like Thrombotic Thrombocytopenic Purpura (TTP) and Hemolytic Uremic Syndrome (HUS) and gene therapy for coagulation disorders like heamophilia A.
A multidisciplinary approach is needed to deal with such cases that involves early detection, prompt treatment, and ongoing care to ensure that the patient live a normal and health life. if you liked this blog and want to know more about the human body go to my website Medrizz.com.
FAQs
What are bleeding and coagulation disorders?
These are conditions where the body’s ability to stop bleeding or form blood clots is impaired, leading to excessive bleeding or unwanted clotting.
What is Idiopathic Thrombocytopenic Purpura (ITP)?
ITP is a disorder where the immune system attacks platelets, leading to low platelet counts and increased bleeding risk.
What is Hemophilia?
Hemophilia is a genetic disorder where the blood doesn’t clot properly due to a deficiency in clotting factors, leading to spontaneous bleeding.
What is Disseminated Intravascular Coagulation (DIC)?
DIC is a condition where abnormal clotting and bleeding occur simultaneously, often due to infections, trauma, or underlying diseases.
Can bleeding and coagulation disorders be cured?
Many disorders can be managed with treatments like medications, transfusions, or plasma exchange, but some, like Hemophilia, are lifelong conditions requiring ongoing care.


1 thought on “Understanding Bleeding and Coagulation Disorders with Causes, Clinical Features and Treatment Options.”